When your dental implants need rejuvenation, understanding the process of restoration of implants is key. This article unpacks the essentials: what contributes to the need for restoration, the procedures involved, and how these techniques aim to deliver longevity and a natural feeling. Without overwhelming detail, we’ll provide a clear path forward for those needing restoration and explain how this process upholds your oral health.
Dental implant restoration offers many benefits beyond aesthetics, including improved function and long-term oral health.
Key Takeaways
- Dental implant restoration comprises three components: the implant fixture, abutment, and prosthetic restoration, which offer a permanent solution for missing teeth and help preserve oral health by preventing bone deterioration and maintaining facial structure.
- The dental implant process involves meticulous planning and precision throughout several stages, from initial assessment and surgical placement to attaching the abutment and crown. The dentist takes careful steps to assess and plan each phase, underlining the need for expert dental professionals to ensure success and longevity.
- Aftercare and maintenance are critical for the longevity of dental implants, requiring investment in professional dental visits for cleanings and early detection of potential issues as well as a daily personal oral hygiene routine.
Understanding Dental Implant Restoration
Dental implant restoration emerges as a saving grace for those grappling with the tribulations of missing teeth. This bespoke solution involves a trifecta of components – the implant fixture, the abutment, and the prosthetic restoration, each tailored to the individual for an enhanced smile reconstruction. Dental implant restoration can replace a missing tooth, restoring both function and appearance by integrating with the jawbone for a natural look and feel. If you’re considering dental implants in Rockville, this advanced approach offers a reliable and personalized path to reclaiming your smile and oral health. Offering a multitude of benefits, dental implant restoration triumphs over other alternatives by ensuring:
- Permanent tooth replacement
- Improved speech
- Seamless chewing
- Preservation of facial structure
- Stabilizing teeth to prevent unwanted shifting.
Restoring a missing tooth with implants can significantly improve self confidence, helping you feel better about your appearance and social interactions.
Defining Implant Restoration
Delving into the heart of dental implant restoration, we uncover the critical role of the implant abutment. This central piece provides a steadfast area for the crown, cementing the bond between the prosthetic tooth and the dental implant. The abutment is used to attach the crown securely to the implant, ensuring stability. With options for cementing or screw retention, flexibility is at the forefront of implant restoration methods.
The abutment screw, pivotal in its role, fastens the abutment and crown together, while an array of materials such as ceramic and zirconium offer a perfect blend of function and aesthetics. Furthermore, in scenarios with limited space, screw-retained crowns become indispensable for their superior retention capabilities.
Importance for Oral Health
The significance of dental implants extends far beyond aesthetics, anchoring themselves as the cornerstone of oral health. By merging with the jawbone, they curtail bone deterioration and even reverse it, thus maintaining the jawbone’s vitality and preventing facial sagging that often accompanies tooth loss. Healthy gums are also essential for the success of dental implants, as they support the healing process and proper integration of the implant with the surrounding tissue.
As anchors in the mouth, implants offer several benefits:
- They stabilize neighboring teeth, preventing potential bite issues and TMJ disorders.
- They improve the appearance of your smile.
- They restore the ability to chew and speak properly.
- They provide long-term oral health and wellbeing.
Embracing dental implants is not just a cosmetic endeavor; it’s a commitment to long-term oral health and wellbeing.
The Anatomy of a Dental Implant
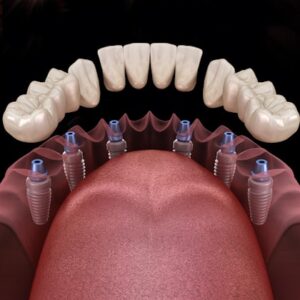
The anatomy of a dental implant is a marvel of modern dentistry, composed of the implant body, the abutment, and the crown. These three parts synergize, creating a structure that is as steadfast as it is visually pleasing.
The dental implant process involves three main components:
- The implant body, often designed as a titanium screw, acts as the root of the replacement tooth and is placed in the jawbone to provide stability and support.
- The abutment serves as the linchpin that secures the crown.
- The crown is the final piece that brings the full effect of a natural tooth to light.
The Implant Body
The implant body, often a titanium alloy, is renowned for its fracture resistance and ability to withstand the rigors of daily mastication without faltering. Its hypoallergenic nature renders it an ideal choice for those with metal sensitivities. Since the 1960s, titanium has been the go-to for dental implants due to its impressive durability and bone-bonding prowess through osseointegration, thus forming a formidable foundation for artificial teeth.
Designed to emulate the root of a natural tooth, the titanium post integrates with the jawbone, often lasting a lifetime thanks to its biocompatibility. These implant posts provide the stable support needed for the final restoration, such as crowns, bridges, or dentures. Endosteal implants, the most frequent type, are meticulously inserted within the jawbone, assuring a reliable base for the restoration to come.
The Abutment Connection
Acting as the intermediary, the abutment forms a crucial connection between the implant body and the prosthetic crown. This component is paramount in supporting the crown, thereby reinforcing the stability and functionality of the entire dental implant restoration.
The Prosthetic Crown
Upon successful fusion of the implant body with the jawbone and the positioning of the abutment, a custom-made implant crown is affixed, completing the dental implant’s transformation. This crown acts as a false tooth, restoring both appearance and function. Crafted to mimic the look and performance of natural teeth, these crowns return full chewing power, often indistinguishable from their natural counterparts by the wearer.
Step by Step: The Dental Implant Restoration Process
The journey to a renewed smile through the dental implant procedure unfolds in a meticulously curated step-by-step process. Beginning with an in-depth dental examination and culminating in the secure attachment of the custom crown, this two-phase journey promises a well-informed and transparent experience for patients, from the initial implant placement to the subsequent restoration phase. After the implant has integrated with the jawbone, a second surgery may be required to place the abutment before the final restoration. This ensures that the restoration process is thorough and complete.
Initial Assessment and Treatment Plan
The odyssey to implant restoration commences with a consult with an expert dentist, who crafts a personalized treatment plan. This initial phase may necessitate tooth extractions and assessments to confirm that the jawbone can support the implant, which could include bone grafting procedures if required. In some cases, an oral surgeon might be involved in these procedures to ensure the best possible outcome.
X-rays and detailed scans are pivotal in planning the precise implant placement, ensuring that the treatment is customized to the patient’s oral health needs and that any potential issues are proactively managed.
Surgical Placement and Healing
The implant’s surgical placement is an outpatient procedure, its complexity contingent upon the implant type and the patient’s jawbone state. The realm of implant surgery boasts advanced techniques like Immediate load dental implants and All-on-4 implants, circumventing bone grafting and facilitating immediate restoration in certain cases. The ensuing osseointegration period, spanning three to six months, is when the jawbone embraces the implant, creating a robust foundation. This process is crucial because it establishes a stable foundation for the final restoration, ensuring long-term durability and functionality.
In some instances, bone augmentation, sinus lifts, or ridge expansions are necessary to bolster the jaw bone for implant support. Post-operative care is paramount, with patients advised to avoid certain activities to ensure proper healing. The precision of implant placement is greatly enhanced by state-of-the-art 3D imaging and surgical planning software, which minimizes procedure time and promotes recovery.
Attaching the Abutment and Crown
Once the implant has successfully united with the jawbone, the abutment is attached, setting the stage for the crown’s placement. This final act in the restoration process involves precise impressions and the delivery of the crown, ensuring that the result is both functional and aesthetically pleasing.
The procedure for zirconium screw-retained crowns, for instance, includes meticulous steps from removing the healing abutment to sealing the screw access channel, all performed with the utmost care to achieve a seamless match with existing dentition.
Addressing Common Concerns in Implant Restoration
Even the most transformative dental procedures come with their set of concerns, and implant restoration is no exception. Potential challenges include:
- Improper implant placement
- Patient non-compliance
- Ramifications of untreated medical conditions
- Implant rejection
- Discomfort or pain around the implant site
Awareness of these issues and how to address them is instrumental in ensuring the success and longevity of the implants, with verification successful waiting being a crucial step in the process.
Managing Soft Tissue and Peri-implant Mucosa
The longevity of a dental implant rests not only on the implant itself but also on the health of the surrounding tissues. Avoiding chronic infections and complications is paramount, and regular professional maintenance, including cleaning and radiographic evaluations, plays a critical role in this endeavor.
Techniques such as the use of non-alcohol rinses and Monoject syringes for cleaning can significantly reduce bacterial load and maintain the health of the peri-implant mucosa.
Preventing and Handling Residual Cement
Residual cement from cement-retained implant restorations can lead to serious complications, including periimplantitis. This issue sheds light on the importance of meticulous cementation techniques and the preference for screw-retained crowns, which allow for easier maintenance and are less prone to causing such complications.
Ensuring Proper Fit and Avoiding Fracture
The integrity of implant restorations largely hinges on ensuring a perfect fit. Misalignment or improper fitting can lead to complications like implant fractures or loosening of the implant crown, which can be both painful and costly to address. A meticulous approach and technical precision are required to avoid such issues, ensuring that restorations are seated completely and securely.
Different Implant Systems and Their Restoration Methods
The world of dental implants is diverse, featuring over 300 different systems, each with its unique restoration methods. Whether one opts for screw-retained or cemented restorations, the choice depends on several factors, including implant angulation and the specific requirements of the patient.
This diversity of implant systems ensures a range of solutions for different dental restoration needs, allowing every individual to find an option that suits their requirements.
Compatibility Across Systems
Restoring an implant is not merely a matter of picking a system; it requires careful consideration of the materials that are compatible with that system. The choice of abutment and crown materials can affect the restoration’s success, making compatibility a key factor in the decision-making process.
Customization for Patient Needs
Customization is the cornerstone of dental implant restoration. Each patient presents a unique set of needs and anatomical considerations, requiring a tailored treatment plan that outlines the number of implants, the type of restoration, and any additional procedures like bone grafting. Treatment plans are carefully designed to address the unique needs of each patient, ensuring optimal results.
This personalized approach is especially important for aesthetic and functional restorations in the visible parts of the mouth.
Advantages and Challenges of Restoring Implants
Restoring implants is not just about filling gaps; it’s about restoring confidence, function, and aesthetics. Maintaining the quality of dental restorations is essential for long-term success. While the advantages like bite stability and jawbone preservation are clear, challenges such as achieving optimal angulation and ensuring technical precision cannot be overlooked. These challenges highlight the need for skilled professionals capable of delivering results that stand the test of time.
Longevity and Durability of Implants
The allure of dental implants lies in their longevity and durability. With proper care, titanium implants can last a lifetime, offering a more enduring solution than alternatives like a bridge or denture, which may require replacement or repair over time.
Additionally, implant-supported dentures, also known as implant prostheses, significantly improve stability and chewing capacity, maintaining their effectiveness far longer than traditional dentures.
Technical Considerations and Skill Level
The technical considerations and the skill level of the dental professional are paramount in the success of implant restorations. In most cases, implant restorations are highly successful and complications are rare. While rare, cases of titanium allergy can present severe complications, emphasizing the need for thorough patient evaluations and expert handling of the implant materials and procedures to ensure a harmonious outcome and minimize the risk of adverse reactions.
Aftercare and Maintenance of Restored Implants

The journey to a flawless smile doesn’t end at the dental chair. Aftercare and maintenance are the unsung heroes in the life of dental implants. Good oral hygiene practices and regular dental check-ups are the bedrock of ensuring that your restored implants remain a source of pride and function for years to come. Regular office visits are essential for monitoring and maintaining restored implants.
Professional Dental Implant Care
The vigilance of professional dental care is the guardian of implant health. Regular check-ups and professional cleanings by a dental hygienist are essential. These visits not only maintain the implant’s integrity but also provide an opportunity for early detection and intervention of potential issues, thereby ensuring the implant’s success over time.
Personal Dental Implant Care
Just as a garden needs daily tending, so do your dental implants require consistent personal care. A daily oral hygiene routine including brushing, flossing, and the use of specialized tools like water flossers, is essential to prevent plaque build-up and safeguard against issues such as calculus formation that can jeopardize the health of the implants.
Cost Factors in Dental Implant Restoration
Dental implant restoration, while a beacon of hope for many, comes with its own set of financial considerations. The cost of dental implant restoration depends on how many teeth need to be replaced, as this directly affects the overall investment. From the cost of a single tooth implant to the more comprehensive All-on-4 dental implant system, the investment varies. However, it’s important to weigh these costs against the long-term benefits and the transformative impact on oral health and lifestyle.
Estimating the Investment
A prudent approach to dental implant restoration involves a clear understanding of the associated costs. The brand of the implant plays a role in the overall expense, with high-end brands often carrying a higher price tag. It’s imperative for patients to consider this when estimating the investment required for their dental transformation.
Comparing Long-Term Value
While the initial expense of dental implants may appear steep, their potential to last a lifetime offers incomparable long-term value. Lower-cost alternatives may seem attractive at first glance, but the durability and benefits of implants often render them a more economical choice in the long run. If a crown or restoration becomes damaged, it can be replaced by a specialist to maintain both function and aesthetics.
Insurance coverage can vary, but it’s worth exploring all financial options to make this life-changing investment more accessible.
Summary
In conclusion, dental implant restoration stands as a testament to modern dental innovation, offering a permanent solution to tooth loss with unmatched benefits in oral health and aesthetics. From the sturdy implant body to the meticulous attachment of the crown, every step of the process is designed to restore function and confidence. Despite the technical challenges and the need for diligent aftercare, the long-term advantages and transformative potential of dental implants make them a worthwhile investment for those seeking to reclaim the fullness of their smile and return to smiling with confidence.
Frequently Asked Questions
What is the expected lifespan of a dental implant?
Dental implants, especially those made from titanium, are designed to last a lifetime with proper maintenance, often outliving other tooth replacement options like dental bridges or traditional dentures. Therefore, the expected lifespan of a dental implant is generally for a lifetime.
Can dental implants be rejected by the body?
Yes, dental implants can be rejected by the body, although it is rare. Rejection can lead to implant failure and may be caused by factors such as allergies to implant materials, infections, or improper placement.
Are dental implants suitable for everyone?
Dental implants are suitable for most people, but a thorough assessment by a qualified dentist is necessary to determine eligibility, taking into account factors like jawbone density, oral health, and medical conditions.
How do I care for my dental implants after the procedure?
To care for your dental implants after the procedure, you should schedule regular professional check-ups and cleanings, while also maintaining a diligent at-home oral hygiene routine consisting of brushing, flossing, and the use of specialized cleaning tools.
Is the cost of dental implant restoration covered by insurance?
Insurance coverage for dental implants varies greatly, and while some plans may cover a portion of the costs, full-mouth restoration treatments like All-on-4 are often not covered. It is advisable to check with your insurance provider for specific coverage details.