Experiencing trouble with dental implants can be concerning. Issues like infection, loose implants, and nerve damage are possible. This article covers these common problems and offers solutions to help you manage them effectively.
Key Takeaways
- Dental implants carry risks such as infection, failure, and nerve damage, necessitating patient awareness and care.
- Early-stage problems can arise within months post-surgery, including infections and bone healing issues that require prompt identification and care.
- Preventative measures, including regular check-ups and choosing an experienced surgeon, are vital for ensuring the long-term success of dental implants.
Common Complications with Dental Implants
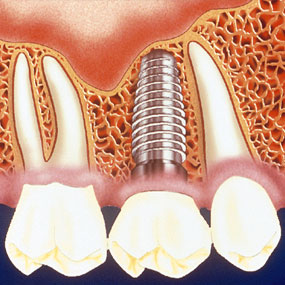
Despite their high success rate, dental implants can pose risks that may affect overall oral health. Common dental implant complications include infection, implant failure, and nerve or tissue damage. These complications can arise from various factors such as poor oral hygiene, surgical errors, or the body’s response to the implant.
Patients should be aware of these potential complications before considering dental implants. Infections at the implant site, loose implants, and nerve or tissue damage are among the most frequently encountered issues. Any of these issues can greatly impact the success of the implant and the patient’s oral health. For a reliable solution, dental implants in Rockville are designed to minimize risks and provide long-lasting results.
Infection at the Implant Site
Infection is a common complication that can occur after dental implant surgery. Symptoms typically include pain, swelling, and drainage from the incision area. Swelling at the implant site, especially with pus formation, can signal an infection that requires urgent attention. Left untreated, infections can lead to severe complications and potentially cause the implant to fail.
Post-surgery infections can often be treated with antibiotics or, in more severe cases, surgical interventions. Proper oral hygiene and adherence to postoperative care instructions help prevent infections.
Early detection and treatment of infections are possible with regular dental check-ups.
Loose Implants
A loose implant is often a sign that something has gone wrong with the osseointegration process, where the implant should fuse with the jawbone. This can occur due to excessive force or impact on the implant, improper planning by the surgeon, or insufficient bone structure to support the implant.
If an implant becomes loose, it may cause difficulty in chewing or biting, indicating that the implant is not properly integrated. In such cases, the implant might need to be removed and the procedure retried once the area has healed.
Adequate bone structure and adherence to dental guidelines help prevent this issue.
Nerve or Tissue Damage
Nerve or tissue damage can occur if the implant is placed too close to a nerve or due to surgical trauma. This can result in symptoms such as numbness, tingling, or persistent pain. These symptoms can sometimes be temporary, but in other cases, they may persist long-term, affecting the patient’s comfort and sensation.
Careful planning and accurate placement are necessary to avoid nerve or tissue damage. Surgeons must be meticulous during the implant procedure to ensure that the implant does not impinge on any nerves or surrounding tissues.
Immediate medical attention is needed for patients experiencing these symptoms.
Early Stage Problems
Early stage problems with dental implants typically occur within the first three to four months after surgery. These issues can include immediate post-surgery infections, bone healing complications, and pain or discomfort. Early identification and treatment of these problems can prevent severe long-term complications.
Improper placement of implants, surgical trauma, or infection can also contribute to these early stage problems. Patients should be vigilant for signs of complications and maintain open communication with their dental care provider during this critical period.
Immediate Post-Surgery Infections
Immediate post-surgery infections are a significant concern and can lead to implant failure if not promptly addressed. Early signs of infection include redness, swelling, and discharge at the implant site. Proper oral hygiene and adherence to postoperative care guidelines can significantly reduce infection risk.
Early detection and timely intervention for infections are facilitated by regular check-ups and symptom monitoring. Antibiotics and careful postoperative care are usually sufficient to treat these infections, but severe cases might require additional surgical intervention.
Bone Healing Issues
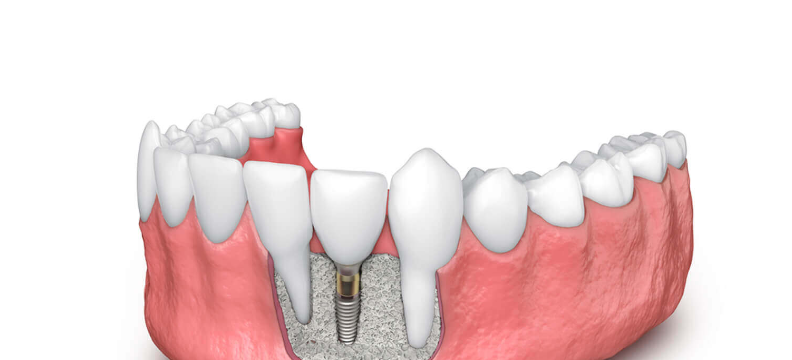
The bone healing process, or osseointegration, is critical for the success of a dental implant. It takes several months for the bone to grow around the implant and stabilize it. However, immediate tooth replacement after implantation can put undue stress on the implant, hindering this process.
If there is insufficient bone to support the implant, it cannot properly fuse with the jaw, leading to instability and potential failure. Bone grafting may be required to support the implant when bone density or quality is insufficient.
Pain and Discomfort
Pain and discomfort are common after dental implant surgery, but they should gradually subside as healing progresses. Patients might experience swelling, tenderness, and sensitivity around the implant area. Ibuprofen or acetaminophen, available over the counter, can help manage this pain.
A cold compress can reduce swelling and numb pain in the affected area. Effective pain and discomfort management ensures a smooth recovery and prompt addressal of potential complications.
Long-Term Complications
Long-term complications from dental implants can arise months or even years after the surgery. These issues include peri-implantitis, gum recession, and sinus problems, each of which can significantly affect the success and longevity of the implant.
Monitoring the implant site and maintaining good oral hygiene are key to preventing long-term issues. Early detection and treatment of emerging problems through regular check-ups ensure the long-term success of the implant.
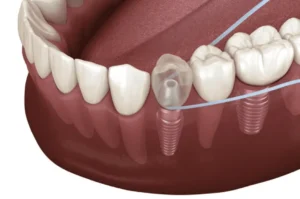
Peri-Implantitis
Peri-implantitis is an inflammation and infection of the tissues surrounding the implant, often caused by poor oral hygiene, smoking, or pre-existing medical conditions. Symptoms include bleeding, swelling, and pain around the implant site. Untreated peri-implantitis can result in bone loss. This may ultimately lead to implant failure.
Effective treatment of peri-implantitis requires early detection and intervention. Treatment focuses on controlling infection, reducing inflammation, and preserving the implant and surrounding bone.
Gum Recession Around Implants
Gum recession around dental implants can lead to inflammation and pain. If not addressed promptly, it can necessitate the removal of the implant. Causes of gum recession include poor oral hygiene, improper implant placement, gum disease, and natural changes in the gum tissue over time.
Preventing gum recession requires regular dental visits and healthy gum maintenance. Immediate assessment by a dentist is necessary if gum recession is noticed, to prevent worsening.
Sinus Problems in Upper Jaw Implants
Dental implants in the upper jaw can sometimes lead to sinus issues, known as sinusitis. Symptoms include sinus inflammation and discomfort. These complications can arise if the implant penetrates the sinus floor or if there is insufficient bone to support the implant.
Oral surgeons use strategies to minimize sinus problem risks during implant placement. Sinus-related complications are rare but can be serious, requiring professional medical attention.
Factors Affecting Implant Success
Regular maintenance and check-ups are vital for the long-term success of dental implants. Early identification and management of risk factors can prevent complications and improve implant success.
Poor Oral Hygiene
Poor oral hygiene is a leading cause of complications after dental implant procedures. Inadequate dental maintenance can adversely impact the success rate of dental implants, increasing the risk of infections and other issues.
Flossing daily and using interdental brushes help maintain the health of the implant and surrounding tissues. Preventing complications and ensuring the longevity of dental implants require regular cleaning and professional dental care.
Smoking and Dental Implants
Smoking significantly increases the risk of dental implant failure due to its adverse effects on circulation and healing. Smokers are advised to quit smoking at least one week before the implant procedure and for two months afterward to improve healing and reduce the risk of complications.
With failure rates reaching up to 20 percent in smokers, quitting smoking is crucial to enhance the chances of a successful implant.
Medical Conditions and Medications
Certain medical conditions and medications can impact the success of dental implants. Systemic health issues like diabetes and autoimmune diseases can severely impede the healing process, preventing proper osseointegration. Slow healing can lead to instability and potential implant failure.
Patients should discuss their medical history with their oral surgeon to develop a treatment plan addressing these risk factors. Managing these conditions properly is vital for the success of dental implants.
Preventative Measures and Solutions

Implementing these measures can help patients avoid common dental implant problems and maintain their overall oral health, ensuring that their investment in dental implants pays off in the long run.
Regular Dental Check-Ups
Monitoring the health and stability of dental implants requires regular dental check-ups. Early detection of potential complications during these visits ensures prompt intervention and prevents severe issues. Consistent check-ups help maintain good oral hygiene, which is vital for the longevity of dental implants.
Dental hygienists provide comprehensive care during check-ups, including professional cleaning and aftercare recommendations. This proactive approach supports both implant health and the patient’s overall oral health.
Proper Aftercare
Proper aftercare is crucial for a smooth recovery after dental implant surgery. Dietary restrictions and activity limitations, as part of post-surgery care instructions, significantly impact the healing process. Patients are advised to avoid hot foods and drinks and stick to a soft food diet to support recovery.
Activities and habits that can affect the healing process should be carefully managed. Following post-surgery guidelines reduces the risk of complications, ensuring proper implant integration with the jawbone and surrounding tissues.
Choosing an Experienced Oral Surgeon
Choosing a qualified and experienced oral surgeon is crucial for the success of dental implants. A skilled surgeon prevents complications during and after the procedure through accurate planning and execution of implant placement. They can foresee potential issues and take preventive measures to mitigate them.
Experienced surgeons can determine the necessary number of implants and tailor the treatment to the patient’s needs. This expertise significantly enhances the likelihood of a successful outcome and long-term satisfaction with dental implants.
Alternatives to Dental Implants
For some patients, dental implants may not be the best option due to medical conditions, bone density issues, or personal preferences. Fortunately, there are alternatives to dental implants that can effectively address missing teeth. Dental bridges and removable partial dentures are two such options that offer different benefits and considerations.
These alternatives can provide functional and aesthetic solutions for tooth replacement without the need for surgical intervention. Knowledge of these options helps patients make informed decisions about oral health and natural teeth replacement.
Dental Bridges
Dental bridges are a common alternative to dental implants, providing a fixed prosthetic solution to fill gaps left by missing teeth. Traditional bridges involve creating crowns for the adjacent teeth and placing a pontic (artificial tooth) in between.
Maryland bridges, on the other hand, use wings attached to the backs of nearby teeth, requiring less alteration of the adjacent teeth. Resin-bonded bridges are another less invasive option, utilizing a special resin to attach the artificial tooth. These bridges can be a suitable choice for patients looking to avoid more extensive procedures while still achieving a functional and natural-looking tooth replacement.
Removable Partial Dentures
Removable partial dentures offer a flexible, non-invasive solution for those missing a few teeth. These dentures are designed to fit over the gums and attach to existing teeth, providing a comfortable and functional replacement.
Compared to dental implants, removable partial dentures are generally more affordable and do not require surgical intervention. However, they do require periodic adjustments to ensure a comfortable fit as oral conditions change. This option allows patients to restore their smile and oral function without undergoing surgery.
Summary

Factors affecting implant success include oral hygiene, smoking, and existing medical conditions. Preventative measures such as regular dental check-ups, proper aftercare, and choosing an experienced oral surgeon can significantly reduce the risk of complications and improve the success rate of dental implants. For those who may not qualify for implants, alternatives like dental bridges and removable partial dentures provide viable options for tooth replacement.
Ultimately, being well-informed and proactive in maintaining oral health are key to ensuring the longevity and functionality of dental implants or any other tooth replacement option. A collaborative approach with dental professionals can help patients navigate their choices and achieve the best possible outcomes for their oral health.
Frequently Asked Questions
What are the common complications associated with dental implants?
Dental implants can lead to complications such as infection, loose implants, and potential nerve or tissue damage. Maintaining proper oral hygiene and carefully following post-operative instructions are crucial to minimizing these risks.
How can I prevent infections after dental implant surgery?
To prevent infections after dental implant surgery, prioritize oral hygiene, adhere to post-operative care instructions, and keep up with regular dental check-ups. Promptly address any signs of infection, like redness or swelling, to ensure a smooth recovery.
What should I do if my dental implant feels loose?
If your dental implant feels loose, you should contact your dental surgeon right away, as this may indicate improper integration that could require further assessment or revision. Prompt attention is crucial to ensure your oral health and the success of your treatment.
Can smoking affect the success of dental implants?
Smoking can severely compromise the success of dental implants by hindering circulation and healing. It is strongly recommended to quit smoking at least one week prior to the procedure and for two months afterward to enhance recovery and minimize risks.
Are there alternatives to dental implants for tooth replacement?
Yes, alternatives to dental implants include dental bridges and removable partial dentures. Both options can effectively replace missing teeth, with dental bridges providing a fixed solution and removable partial dentures offering flexibility.