Oral surgery dental treatments can be life-changing, improving oral health, function, and appearance for many patients. From wisdom teeth removal to dental implants, oral and maxillofacial surgeons play a vital role in the field of dentistry.
Are you curious about the different types of oral surgery dental procedures, their benefits, and what to expect during the process? This comprehensive guide will provide you with essential information on the role of oral and maxillofacial surgeons, common procedures, and how to prepare for and recover from your oral surgery dental appointment.
Key Takeaways
- Oral and maxillofacial surgeons are highly trained dental specialists who possess extensive education, training, and expertise in performing complex oral surgeries.
- Oral surgery dental procedures encompass a range of treatments to improve oral health including tooth extractions, periodontal surgery and orthognathic surgery.
- Benefits include improved oral health, function, appearance as well as quality of life for those seeking to enhance their wellbeing.
The Role of Oral and Maxillofacial Surgeons in Dentistry
Oral and maxillofacial surgeons, also known as oral surgeons, are dental specialists integral to the field of dentistry. They perform complex oral surgeries and administer anesthesia, ensuring patient comfort during procedures. These highly skilled professionals possess extensive education, training, and expertise, distinguishing them from general dentists.
They primarily focus on the following procedures:
- Extraction of diseased or impacted teeth
- Surgical exposure of impacted teeth
- Preparation of the mouth for dentures
- Treatment of oral infections
- Biopsy of suspicious lesions of the hard and soft tissue
In addition, they also treat facial injuries such as fractures and reconnect severed nerves and ducts.
Education and Training
The path to becoming an oral and maxillofacial surgeon is paved with intense education and training. These specialists complete dental school, followed by at least four years of hospital-based surgical residency training to gain proficiency in treating the teeth, jaw, and facial areas around the mouth with oral and maxillofacial surgery.
To become board certified, oral and maxillofacial surgeons must fulfill a stringent certification process that entails:
- Verification of educational attainment
- Licensure
- References
- Successful completion of comprehensive examinations
The depth of their training and education distinguishes oral and maxillofacial surgeons from general dentists.
Scope of Practice
Oral and maxillofacial surgeons specialize in a wide range of surgical procedures, from tooth extractions to facial reconstruction. Their scope of practice encompasses the entire maxillofacial complex, including bony and soft tissue reconstruction of the entire maxillofacial skeleton.
Apart from standard procedures, oral and maxillofacial surgeons may also be responsible for:
- Preparing the mouth for dentures
- Treating oral infections
- Biopsying suspicious lesions of the hard and soft tissue
- Performing cleft and craniofacial surgery for the correction of congenital and acquired defects of the maxillofacial region, such as cleft lip and palate
Their expertise extends to a wide range of procedures and treatments.
Anesthesia Expertise
The administration of anesthesia is a key forte of oral and maxillofacial surgeons. They possess an in-depth knowledge and proficiency in patient evaluation, anesthesia technique, patient monitoring, and attaining the desired level of anesthesia. Anesthesia options utilized in oral surgery include nitrous oxide, oral medications, or intravenous (IV) moderate or deep sedation.
For example, orthognathic surgery is a surgical procedure performed typically under general anesthesia. This expertise ensures patient comfort and safety during surgical procedures.
Types of Oral Surgery Dental Procedures
There are several common types of oral surgery dental procedures, including:
- Tooth extractions
- Dental implants
- Periodontal surgery
- Orthognathic surgery
These procedures significantly contribute to resolving diverse dental issues and enhancing overall oral health at a dental office.
Each procedure has its unique purpose and indications, ranging from removing impacted teeth to correcting jaw misalignments.
Tooth Extractions
Tooth extractions are one of the most widespread types of oral surgery, often performed to address significant tooth decay, periodontitis, dental trauma, or complications with wisdom teeth. The extraction procedure involves numbing the tooth, extracting it from the socket, controlling bleeding, and closing the space left by the tooth.
Recovery generally spans a few days, throughout which patients are encouraged to medicate pain, avoid strenuous activities, and stick to a soft food diet.
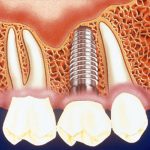
Dental Implants
Dental implants are a popular solution for replacing missing teeth. These titanium metal cylinders act as replacements for tooth roots, providing a stable foundation for artificial teeth.
Oral and maxillofacial surgeons are responsible for:
- Planning and placing dental implants
- Ensuring successful tooth replacement and improved oral function
- Training for the placement of implants involves accurate diagnosis and treatment
- Site preparation, which consists of reconstruction of bone and soft tissues
- Providing maintenance
Periodontal Surgery
Periodontal surgery is a procedure used to treat moderate to severe cases of periodontitis, a serious gum infection that can lead to damage to the soft tissue and bone that support the teeth. This type of surgery involves gum grafts, bone grafts, or pocket reduction procedures to restore gum health and prevent tooth loss.
Successful recovery heavily relies on proper post-operative care, which involves dietary adherence and maintaining good oral hygiene.
Orthognathic Surgery
Orthognathic surgery, commonly referred to as jaw surgery, is a surgical procedure that corrects irregularities and misalignments of the upper jaw (maxilla) and lower jaw (mandible). This procedure involves repositioning the jaws to improve both their form and function.
Indications for corrective jaw surgery may include enhancing mastication, rectifying misalignment, or addressing facial asymmetries. Although potential risks and complications may include infection, dry socket, and nerve injury, many patients experience significant improvements in jaw function and appearance following orthognathic surgery.
Indications for Oral Surgery Dental Treatments
Certain dental issues may necessitate oral surgery dental treatments, such as impacted teeth, severe gum disease, and facial injuries. These conditions often require the specialized skills and expertise of oral and maxillofacial surgeons to ensure successful treatment and recovery.
Impacted Teeth
Impacted teeth, such as wisdom teeth, occur when a tooth is lodged in the jawbone and unable to erupt in the usual manner. In some cases, surgical removal of impacted teeth may be necessary to prevent complications like infection, dry socket, and nerve injury.
For a smooth recovery, proper post-operative care is indispensable, encompassing pain management, swelling reduction, and compliance with dietary restrictions.
Severe Gum Disease
Severe gum disease, or periodontitis, is a serious gum infection that can lead to damage to the soft tissue and bone that support the teeth. Periodontal surgery may be necessary in cases where gum disease has progressed to severe levels, resulting in gums receding from the teeth, bone loss, and loosening or loss of teeth.
Adhering to a strict oral hygiene regimen, including brushing and flossing daily and scheduling regular check-ups and cleanings with a dentist, is the most effective way to prevent tooth loss due to severe gum disease.
Facial Injuries
Facial injuries, including fractures, cuts, and burns, may require oral surgery for proper healing and reconstruction. Oral and maxillofacial surgeons are equipped to treat facial injuries, ranging from routine to complex. They are capable of setting fractured jaw and facial bones as well as reconnecting severed nerves and ducts..
Prompt medical attention is essential to accurately assess and treat facial injuries.
Preparing for Your Oral Surgery Dental Appointment
To prepare for your oral surgery dental appointment, it’s necessary to follow a few key steps including adhering to pre-operative instructions, sorting out transportation, and discussing anesthesia options with your oral surgeon.
Proper preparation ensures a smooth procedure and promotes a successful recovery.
Pre-operative Instructions
Before your appointment, it is imperative to adhere to your oral surgeon’s pre-operative instructions. These instructions may include fasting for a specified duration, abstaining from certain medications, and informing your surgeon of any allergies or medical conditions.
Adhering to these instructions guarantees a safe and successful procedure.
Transportation Arrangements
Given that anesthesia may affect your driving ability, arranging for a responsible adult to chauffeur you to and from your appointment is a necessity.
Alternatively, you can take a cab, Uber, or use public transportation to ensure your safety and the safety of others on the road.
Anesthesia Options
Anesthesia options for oral surgery dental procedures include local anesthesia, conscious sedation, and general anesthesia. Discussing these options with your oral surgeon before the procedure will help you choose the most suitable type of anesthesia to ensure your comfort during the surgery.
Each type of anesthesia has its own advantages and disadvantages, so it is important to understand the
Post-Operative Care and Recovery
Following your oral surgery dental procedure, successful outcomes heavily rest on proper post-operative care and recovery. Managing pain, reducing swelling, and adhering to dietary restrictions are essential steps to take during your recovery period.
Pain Management
Post-procedure pain management is crucial to ensure a comfortable recovery following your oral surgery dental procedure. Your oral surgeon may prescribe medications to help alleviate pain, or recommend over-the-counter pain relievers.
Additionally, applying ice to the area, consuming soft foods, rinsing with warm salt water, and taking it easy can help manage pain and promote healing.
Swelling Reduction
Reducing swelling is a crucial part of the recovery process. Apply cold compresses or ice packs to the affected area for the first 24 hours, following the 15-minute on and 15-minute off intervals throughout the day.
Keeping your head elevated can also help reduce swelling and promote healing.
Dietary Restrictions
Adherence to dietary restrictions post-procedure is pivotal for a smooth recovery following your oral surgery. Consume soft foods, avoid hot foods and beverages, and select nutrient-rich foods for optimal healing.
Additionally, avoid using straws, as the suction can dislodge blood clots and delay healing.
Potential Risks and Complications
Despite oral surgery dental procedures being generally safe, potential risks and complications such as infection, dry socket, and nerve injury should not be overlooked.
Being informed about these risks can help you take the necessary precautions and seek medical attention if needed.
Infection
Infection is a common complication of oral surgery dental procedures, occurring when bacteria enter the surgical site and cause inflammation and swelling. Following post-operative instructions and maintaining good oral hygiene can help minimize the risk of infection.
If you experience signs of infection, such as increased pain, swelling, or fever, contact your oral surgeon or dentist immediately.
Dry Socket
Dry socket is a painful condition that occurs when the blood clot that forms after a tooth extraction fails to form or is dislodged, resulting in pain, swelling, and infection.
To prevent dry socket, refrain from smoking and adhere to dietary guidelines provided by your oral surgeon.
If you suspect dry socket, seek prompt medical attention for proper treatment.
Nerve Injury
Nerve injury is a rare complication of oral surgery dental procedures that occurs when the nerves in the jaw are damaged during the procedure. This can result in numbness, tingling, or pain in the affected area.
Most nerve injuries recover within six to eight weeks with appropriate management and treatment, but if the effects persist for more than six months, the nerve damage may be permanent. Seek prompt medical attention if you experience any nerve-related symptoms after your oral surgery.
When to Consult with Your Oral Surgeon or Dentist
If you experience persistent pain, swelling, or other worrisome symptoms following your oral surgery dental procedure, consulting with your oral surgeon or dentist is of utmost importance. Early intervention can help prevent complications and promote proper healing.
Remember, your oral surgeon or dentist is there to support you throughout your recovery and ensure a successful outcome.
The Benefits of Oral Surgery Dental Treatments
Oral surgery dental treatments boast numerous advantages, such as:
- Enhanced oral health
- Improved function
- Enhanced appearance
- Elevated quality of life
From addressing impacted teeth to treating severe gum disease, these procedures provide life-changing solutions for patients.
Whether you’re considering oral surgery for yourself or a loved one, understanding the benefits and the process can help you make an informed decision and achieve the best possible outcome.
Summary
In summary, oral surgery dental treatments play a vital role in ensuring optimal oral health and improving the quality of life for many patients. From tooth extractions to dental implants, these procedures address a wide range of dental issues and are performed by highly skilled oral and maxillofacial surgeons. With proper preparation, post-operative care, and adherence to your oral surgeon’s instructions, you can experience a successful outcome and enjoy the benefits of improved oral health, function, and appearance.
Frequently Asked Questions
What is the difference between dental surgery and oral surgery?
Oral surgeons provide more complex surgical care than dentists, such as wisdom tooth extraction and reconstructive dental surgery following an accident. Oral surgeons are also more likely to be equipped with anesthesia options for surgical procedures.
Are you put to sleep for oral surgery?
Yes, you will sometimes be put to sleep for oral surgery. This is done to ensure you don’t feel any pain or discomfort during the procedure.
What are the most common types of oral surgery dental procedures?
Common types of oral surgery dental procedures include tooth extractions, dental implants, periodontal surgery, and orthognathic surgery.
How can I prepare for my oral surgery dental appointment?
Prior to your appointment, follow pre-operative instructions, arrange transportation, and discuss anesthesia options with your surgeon to ensure a successful surgery and recovery.
What are some potential risks and complications of oral surgery dental procedures?
Potential risks and complications of oral surgery dental procedures include infection, dry socket, and nerve injury.