When the jawbone isn’t sturdy enough for a dental bone graft implant, a dental bone graft becomes necessary. This procedure rebuilds bone, offering the solidity needed for a dental implant. Our guide will take you through why bone grafts are essential, what the surgery involves, and how to navigate the process for optimal healing and success. Expect insights into post-operative care, potential complications, and the long-standing benefits that make the procedure worthwhile, without delving into the specifics just yet.
Key Takeaways
- Dental bone grafting is essential for implant success, serving as the sturdy foundation required for implants by replenishing lost bone through materials such as autografts, allografts, and xenografts.
- Preparation for dental bone graft implant surgery includes a comprehensive assessment of oral health, bone density, and volume, followed by a personalized treatment plan to ensure optimal outcomes.
- The grafting procedure is meticulously carried out in a series of steps including site preparation and the placement of bone graft material, followed by monitoring and care post-surgery to secure successful bone healing and implant integration.
Understanding Dental Bone Grafts and Implants

The catalysts for bone grafting often stem from tooth extraction, gum disease, or injury, which lead to bone loss. Dental implants then step onto the stage, offering solid support for new teeth, effectively mirroring the strength and function of natural teeth. Synthetic bone grafts play a crucial role in this two-part symphony of grafting and implants, restoring not just the physical form, but the symphonic harmony of a full, vibrant smile.
The Role of Bone Grafting in Dental Implant Success
Bone grafting takes center stage due to its pivotal role in ensuring the success of dental implants. It’s the architect that restores volume to the jawbone, ensuring it’s primed for the structural demands of implants. Without adequate bone density, our jawbone would be like a stage without a spotlight, unable to support the star performer—the dental implant. For those considering dental implants Rockville MD, bone grafting is often a crucial first step in preparing the jawbone. Beyond the limelight, bone grafting is also the unsung hero in reconstructive surgeries, especially after facial trauma, by restoring symmetry and bone volume. Bone grafting surgery helps maintain proper tooth alignment, thwarting the domino effect of jawbone resorption that could otherwise lead to a cascade of complications.
Investing in bone grafting equates to investing in one’s future oral function. It’s a proactive step towards ensuring that the oral cavity remains a well-tuned orchestra, capable of performing the daily symphony of eating, speaking, and smiling without a hitch.
Key Materials Used in Bone Grafting
In the realm of dental bone grafting, the materials used are as varied as the instruments in a philharmonic orchestra, each contributing its unique timbre to the overall success. Some of the materials used include:
- Autografts: the gold standard, using the patient’s own bone to encourage seamless integration and harmony within the jaw
- Allografts: sourced from human donors, offering their bone material when the patient’s own is unavailable
- Xenografts: with calcified matrices from bovines, providing an alternative when human bone is unsuitable
These different materials serve different purposes and are used based on the specific needs of each patient.
The members of this ensemble include:
- Natural bone, which serves as the foundation and main support for the dental implant
- Dental implants, which act as the anchors for the replacement teeth
- Abutments, which connect the dental implants to the replacement teeth
- Crowns, bridges, or dentures, which are the replacement teeth that are attached to the dental implants
Together, these materials create a symphonic blend that supports and encourages new bone growth, setting the stage for a dental implant’s successful placement.
Preparing for Dental Bone Graft Implant Surgery

With insights in hand, a personalized treatment plan is crafted, detailing the nuances of the dental bone graft procedure. This plan is akin to a musical composition, tailored to suit the patient’s unique oral health needs and the intricate choreography required for a flawless dental surgery.
This preparation phase isn’t only about getting the stage ready; it also ensures that the patient takes an informed and active role in the decision-making process. After all, a successful outcome relies on a partnership between patient and practitioner, much like a duet between a pianist and a violinist, each contributing to the creation of beautiful music.
Assessing Bone Density and Volume
Before the surgical act begins, a critical assessment of our jawbone is carried out. Dental X-rays and scans are the high-definition cameras capturing every contour and angle of the bone, revealing the story of bone loss and the current density and volume. This step ensures that the stage is set for success, ready to support the high demands of a bone graft and, eventually, the star of the show—a dental implant. It’s a vital prelude to the procedure, guaranteeing the foundation is solid enough for the jawbone to play its supporting role without faltering.
Customizing the Treatment Plan
Just as every individual is a unique mix of experiences and genetics, the treatment plan for dental bone grafting must also be personalized. It’s a collaborative process, akin to a composer tweaking a score in harmony with a soloist’s style. The options for the dental bone graft are laid out before the patient, ensuring a well-informed decision that harmonizes with their distinct oral health needs and the desired outcome for bone volume and quality.
This bespoke approach to treatment planning is the key to orchestrating optimal outcomes, ensuring that each patient’s journey towards implant surgery is as smooth and successful as the most captivating of arias.
Step-by-Step: The Dental Bone Graft Implant Process

An incision in the gum tissue reveals the jawbone, akin to the opening act where the stage is set for the bone graft material to make its entrance. The graft is then meticulously placed and secured, much like a soloist taking position center stage, ready for a virtuoso performance.
Finally, the surgical site is closed with the finesse of a final curtain call, marking the end of the initial act. This procedure is not just a series of mechanical steps, but a deliberate and artful dance between the surgeon and the patient’s oral landscape. Each move is calculated to ensure successful graft integration and the ultimate placement of the dental implant.
Surgical Site Preparation
The surgical site preparation includes the following steps:
- An incision is made in the gums, gently parting the tissue to unveil the bone beneath.
- The site is then meticulously cleaned, removing any debris or bacteria.
- The bone graft material is then applied to the site, setting a pristine stage for the bone regeneration process.
These steps ensure that the surgical site is properly prepared for the bone graft procedure.
This step is fundamental, ensuring that the foundation is ready to welcome the graft material and support the dental implant’s future performance.
Placing the Bone Graft Material
With the spotlight now on the jawbone, the surgical suite becomes a stage where precision and care are paramount. The bone graft material, the protagonist of our narrative, is placed with exactitude in the prepared area, ensuring a perfect fit within the existing bone structure. This placement is not simply about filling a void; it’s about setting the groundwork for new bone growth, creating a stable foundation that will support the coming attractions—the dental implants. The transplanted bone, in this case, plays a crucial role in the overall success of the procedure.
The material is secured, much like an anchor holding a ship steadfast amidst turbulent seas, guaranteeing stability and promoting successful bone healing by supporting the bone tissue.
Ensuring Successful Bone Healing
After placing the bone graft, the focus shifts to creating a healing-friendly environment. A resorbable membrane may be placed over the graft site, acting as a protective shield while the body orchestrates the complex symphony of bone regeneration. The patient is advised to keep their head elevated, a simple yet effective measure akin to holding a note to ensure the swelling fades gracefully.
Vigorous rinsing, which could disrupt the delicate new composition of tissue and bone, is to be avoided, ensuring the blood clot—much like the audience at a performance—remains undisturbed. Over the following three to nine months, the stage is set for complete healing, a period of intermission where the body’s natural processes work their magic to prepare for the grand finale: the placement of the dental implant.
Post-Operative Care: Ensuring Optimal Healing

Small fragments, much like the stray notes of a rehearsal, may appear at the graft site, signaling the body’s adaptation and healing. A balanced diet, soft and rich in nutrients, becomes the patient’s repertoire, supporting the body’s natural healing process. Antibiotics may be prescribed as a preventative measure against infection, and pain relievers help manage discomfort, ensuring the patient’s comfort and peace of mind.
Within one to two weeks, patients typically feel back to their normal selves, although the complete symphony of recovery plays out over a unique time frame for each individual.
Managing Pain and Discomfort
The recovery intermezzo may feature pain and swelling, which are inevitable but manageable aspects of the healing process. Prescribed pain relievers, alongside the simple yet effective application of cold compresses, provide relief, allowing patients to rest and recuperate with ease.
It’s a period of gentle care, where each patient is the soloist, and comfort is the ultimate goal.
Dietary Adjustments and Oral Hygiene
In the days following surgery, patients are advised to adopt a soft food diet that won’t disturb the healing graft, providing gentle nourishment. This dietary interlude, rich in vitamins and minerals, aids in the body’s restorative process, much like a soothing melody that aids in relaxation.
Post-operative care includes:
- Saltwater rinses or prescribed antimicrobial mouthwashes to ensure the oral cavity remains a sterile environment.
- Avoidance of straws to prevent disturbance of the graft.
- Gentle brushing of teeth to maintain oral hygiene and prevent disruption of the graft.
These measures ensure the graft remains undisturbed and on track for a successful crescendo.
Over time, as the harmony of healing progresses, solid foods are reintroduced, allowing the patient to gradually return to the full symphony of flavors and textures they once enjoyed.
Follow-Up Visits and Monitoring Progress
Regular follow-up visits maintain the recovery tempo, much like a series of rehearsals preceding a grand performance. The oral surgeon, acting as the conductor, carefully monitors the healing of the dental bone graft and readies the patient for the next stage: implant placement. These check-ups are instrumental, ensuring that the graft is not only healing but thriving, ready to support the future dental implants.
Any signs of discomfort or inflammation are addressed, ensuring that the patient’s journey to restored oral health continues without discord.
Timing and Placement of Dental Implants After Bone Grafting

In cases where the jawbone is healthy and resilient, the dental implant can take center stage as soon as 2 months after the graft. However, for most patients, the bone graft material needs time to mature into sturdy bone—a process usually lasting between 3 to 6 months—before the implant surgery can be scheduled. When the graft is of a moderate size, the interlude can be as brief as 3 to 6 months, while a more significant loss may require an extended period of up to 6 to 9 months of healing before the implants can be placed.
This interval is not merely a pause; it is a period of anticipation, where the body meticulously crafts new bone in preparation for the dental implants. Much like the meticulous tuning of an instrument before a solo, this time ensures that when the implants are placed, they will be in perfect harmony with the jawbone, providing a lifetime of stability and function.
Understanding Osseointegration
Osseointegration, the process where the jawbone and the implant unite to form a strong and resilient bond, is the cornerstone of dental implant success. It’s the intricate dance of bone cells growing into and uniting with the implant’s surface, a biological performance that requires a solid and healthy foundation provided by the bone graft. The graft not only supports the implant but also promotes successful osseointegration, ensuring the implant’s stability is as enduring as a timeless melody.
The processes of osteoinduction and osteogenesis play their parts in this biological concerto, with osteoprogenitor cells transforming into bone-building osteoblasts and contributing to the growth of new bone around the implant. Understanding this complex interplay is crucial for patients as it underscores the importance of the bone grafting process and the role it plays in the longevity of dental implants.
Scheduling the Implant Surgery
As the final act in the dental restoration process approaches, the decision to schedule the implant surgery is akin to the careful timing of a conductor’s baton. The ideal window for this appointment is typically within 3 to 6 months post-grafting, allowing for the full maturation of the graft into robust bone. This window ensures that the implant will be placed on a stage of strength, set for optimal integration and the best chance of a standing ovation from the patient’s oral cavity.
For the grand finale of osseointegration to proceed without a hitch, it’s recommended that implant placement occurs within six to twelve months following the bone graft. This meticulous planning and timing are the crescendos to the symphony of dental restoration, ensuring a lasting and harmonious result.
Potential Complications and How to Address Them

To minimize the risk of complications such as excessive bleeding, patients should avoid strenuous activities and adhere to care instructions that promote proper healing. Should severe complications like dental bone graft failure occur, the corrective measures can be as extensive as removing the implant, cleaning the bone, and reattempting the procedure after a period of healing, while bone graft rejection might necessitate corrective surgery or immunosuppressive medications.
Recognizing Signs of Infection or Rejection
Being aware is the first line of defense against potential complications. Patients must stay attuned to their body’s healing symphony for any discordant notes that suggest infection or rejection. Here are some telltale signs that may indicate an infection or the body’s refusal of the graft:
- Worsening pain or swelling after the initial week
- Pus or drainage from the graft site
- Gum recession
- A lack of improvement in jawbone volume
If you experience any of these symptoms, it is important to consult with your healthcare provider as soon as possible.
Recognizing these symptoms early is critical, as they may lead to the failure of the dental bone graft if unaddressed. Timely intervention is essential for the success of the procedure, much like how a quick adjustment can save a musical performance from going awry.
Strategies for Preventing Implant Failure
The success of a dental implant requires careful orchestration, with prevention playing a key role in avoiding implant failure. Lifestyle choices can significantly influence outcomes. Here are some tips to ensure a successful dental implant:
- Avoid smoking, as it is a known antagonist to implant success.
- Eschew tobacco and alcohol during the early post-operative period to ensure the graft and future implant are not compromised.
- Follow your dentist’s instructions for post-operative care to promote a successful healing process.
By following these tips, you can increase the chances of a successful dental implant.
These strategies are not merely suggestions but critical measures in the grand composition of dental restoration, ensuring that each note of the patient’s journey towards a revitalized smile is pitch-perfect.
The Long-Term Benefits of Dental Bone Graft Implants
Beyond the immediate success of dental bone graft implant procedures is a future filled with benefits. A stable foundation for dental implants is just the prelude to a symphony of long-term advantages that unfold over time. The restored bone structure is not only essential for implant support but also for the holistic health of the oral cavity, much like a strong backbone is vital for the overall well-being of the body. Some of the long-term benefits of dental bone graft implant procedures include:
- Improved chewing and speaking ability
- Enhanced facial appearance and self-confidence
- Prevention of further bone loss in the jaw
- Preservation of adjacent teeth
- Long-lasting and durable results
These benefits make dental bone graft implant procedures a worthwhile investment for patients seeking a permanent solution to a missing tooth.
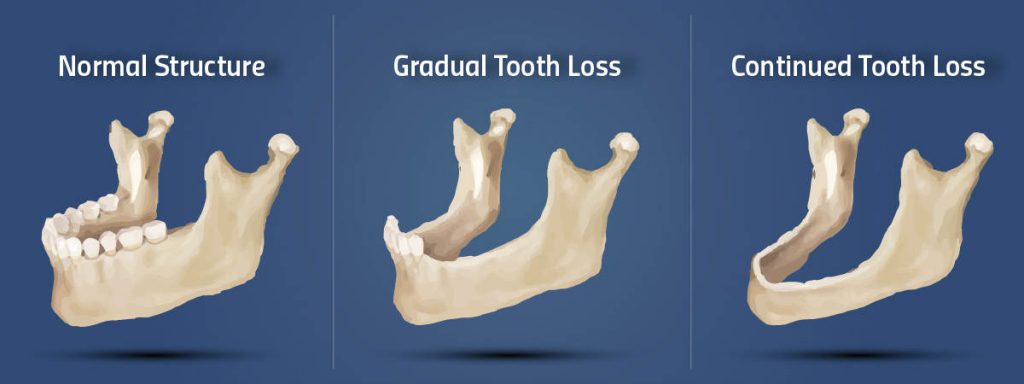
Improved oral function, such as enhanced chewing and speaking abilities, is a significant benefit, allowing patients to indulge in life’s simple pleasures once again. Additionally, the preservation of bone structure through grafting contributes to maintaining the natural contours of the face, preventing the sunken appearance that can occur with significant tooth and bone loss.
Restoring Full Dental Functionality
The pinnacle of dental bone grafting is the restoration of full dental functionality, which brings the mouth back to its full potential. The integrity of the jawbone is reinforced, enabling robust chewing function and clear enunciation, much like a well-tuned instrument enables a flawless performance.
Overall mouth health is revitalized, and the natural structure of the jawbone is preserved, preventing the deterioration of adjacent teeth and supporting healthy gum tissue. This rejuvenated functionality allows individuals to engage confidently in the everyday concerto of eating, speaking, and smiling, each action resonating with the joy of regained health.
Enhancing Facial Structure and Appearance
The aesthetic benefits of dental bone grafts include:
- Maintaining the jawbone’s natural shape and structure, preventing the hollow look that can accompany tooth and bone loss
- Preserving facial contours
- Providing support for prosthetic teeth, contributing to an improved smile and enhancing the patient’s overall appearance.
This solid foundation not only supports the prosthetics but also plays a crucial role in maintaining the integrity of the facial structure, ensuring that the patient’s visage continues to reflect their inner vitality.
Summary
In conclusion, the journey through dental bone graft implant procedures is akin to a masterfully composed piece of music, each phase contributing to the final, harmonious outcome. From the initial assessment and choice of graft materials to the meticulous surgical process and diligent post-operative care, every step is crucial in ensuring the success and longevity of dental implants. The potential for complications exists but can be expertly managed with the right strategies and awareness. Ultimately, the long-term benefits of restored functionality and enhanced aesthetics play a resounding chord in the lives of patients, offering a renewed sense of confidence and well-being. Embrace the process, and look forward to the transformative results that await at the end of this intricate dental symphony.
Frequently Asked Questions
How long does it take for the bone graft to heal before dental implants can be placed?
Bone grafts typically require a healing time of 3 to 6 months before dental implants can be placed, which depends on the individual’s healing process and the size of the graft.
Can I eat normally after a dental bone graft procedure?
After a dental bone graft procedure, it’s best to stick to a soft food diet initially to avoid disturbing the graft site. As the graft heals, solid foods can gradually be reintroduced based on comfort and healing progress.
Are there any activities I should avoid after getting a bone graft?
Yes, it’s advised to avoid strenuous activities, smoking, and alcohol consumption for at least the first two weeks after a bone graft to promote proper healing.
What are the signs of bone graft failure or rejection?
If you experience worsening pain, swelling, pus or drainage at the graft site, gum recession, or a lack of improvement in jawbone volume, it may indicate bone graft failure or rejection. It is important to seek prompt medical attention if these signs occur.
How do I know if my bone graft is healing correctly?
You can gauge the success of your bone graft by observing reduced pain, swelling, and improved jawbone volume, and it’s important to attend regular follow-up visits with your oral surgeon to monitor the healing process.