Need a dental implant and wondering about bone grafts? Bone grafts in dentistry are essential for patients who lack the jawbone structure necessary for implant support. This article unpacks the role of bone grafts in providing a solid base for implants and examines the types used in dental restoration. With a clear focus on their significance and application, you’ll understand how they contribute to the durability and success of your dental work.
Key Takeaways
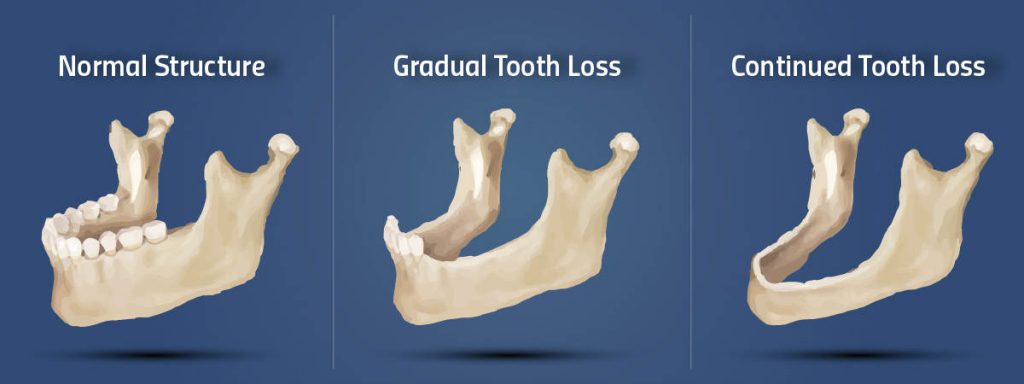
- Dental bone grafts are essential for reconstructing jawbone defects, offering a stable foundation for dental implants and preventing bone resorption, which is critical for maintaining oral health and retaining facial profiles.
- There are four primary types of dental bone graft materials: autografts (patient’s own bone), allografts (human donor bone), xenografts (animal bone), and alloplastic grafts (synthetic materials), each with specific applications and associated risks.
- The dental bone grafting procedure is complex, requiring careful pre-procedure assessment, precise surgical techniques, and an extensive recovery period that varies by individual’s healing capacity and graft type, with potential risks of infection, nerve damage, and failure, especially in smokers.
Understanding Dental Bone Grafts: Purpose and Benefits

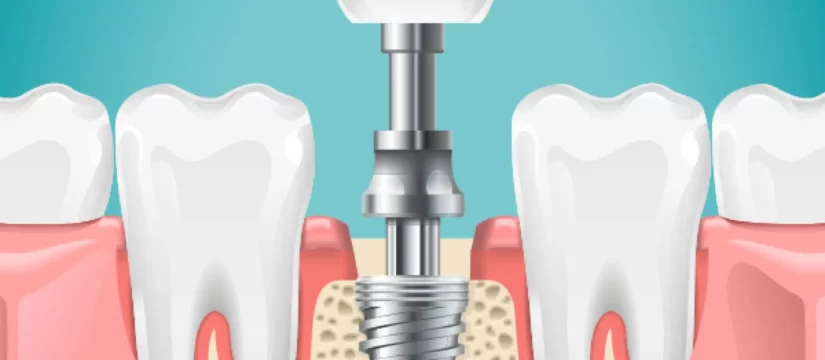
Grafts, once integrated with the jawbone, enhance the stability of dental implants by:
-
Leveraging the bone growth and fusion promoted by osseointegration
- Preventing natural bone resorption in the jaw after tooth loss
- Preserving the stability of remaining teeth
- Retaining the facial profile
-
Maintaining overall oral health.
The Role of Bone Grafts in Dentistry
In the dental field, bone grafts have a fundamental role in halting and reversing bone deterioration, particularly in areas affected by gum disease. This is achieved by using healthy transplanted bone tissue or alternatives like FDA-approved osseous powder or synthetic dental bone. The surgical bone grafting procedure stimulates the body to produce new, healthy osseous tissue, which is necessary to support dental implants or natural teeth.
In addition, guided tissue regeneration is employed in association with bone grafting. This method utilizes barrier membranes to encourage growth of bone and periodontal tissues in areas where bone volume is deficient. In treating periodontal intrabony defects, bioactive glass is used to promote the initiation of mineralized bone formation.
Advantages of Bone Grafting
Dental bone grafts are instrumental in successful oral rehabilitation, owing to their high success rates and the integral role they play in guaranteeing the longevity of dental implants. When a patient’s natural bone is insufficient, bone grafting becomes essential, creating a stable foundation for dental implants and subsequent dental restorations.
The procedure prevents bone loss in the jaw, a common issue after tooth extractions, by providing necessary support to the dental structures. Moreover, bone grafting expands treatment possibilities by offering alternative solutions for patients with inadequate bone height and those seeking alternatives to cumbersome dentures.
Types of Dental Bone Grafts: Materials and Sources
There are four main categories of dental bone grafts: autografts, allografts, xenografts, and alloplastic grafts. Each type has unique sources and properties, making them suitable for different dental applications.
There are three main types of bone grafts:
- Autografts: Utilize the patient’s own bone tissue, typically harvested from another part of their body.
- Allografts: Derived from another human, which can be a living donor or cadaveric bone sourced from a tissue bank.
- Xenografts: Use bone material from animals, commonly cows or pigs, especially in situations where human bone is not available in sufficient quantities.
Regardless of their type, all bone graft materials are sterilized to prevent the transmission of infectious diseases.
Autografts
Autografts necessitate the extraction of bone from the patient’s body for use in bone grafting procedures. The surgeon harvests bone from another area within the patient’s body, ensuring a perfect genetic match and reducing the risk of rejection.
Autografts are particularly used in critical dental cases such as:
- Jaw reconstruction
- Congenital bone defects
- Tumors
- Bone defects larger than 5 mm
Utilizing their osteoinductive and osteogenic properties, autografts offer excellent biocompatibility and healing potential.
Allografts
Allografts incorporate bone from a deceased donor, which is sanitized to minimize the risk of disease or bacterial transmission. They are typically sourced from bone banks where donated bones are processed and stored for medical use.
Dental allografts can be categorized as:
- Fresh
- Fresh-frozen
- Demineralized freeze-dried bone allograft (DFDBA)
- Freeze-dried bone allograft (FDBA)
The preparation of DFDBA involves the removal of mineral content from the bone, using a demineralizing agent, to leave behind osteoinductive agents in a demineralized bone matrix. Despite their benefits, allografts carry risks such as immune rejection and potential disease transmission.
Xenografts
Xenografts, a kind of bone graft material, are typically derived from animals and frequently utilized in dental procedures. Dentists favor xenografts for their osteoconductive properties which facilitate bone growth, and because their chemical composition closely resembles that of human bone.
Despite their benefits, xenografts in dentistry raise certain ethical and health concerns that must be considered. It’s crucial for patients to be informed of these factors and to discuss any concerns with their dental professional before proceeding with a xenograft.
Alloplastic Grafts
Alloplastic grafts are constructed from synthetic materials, designed to replicate the properties of natural bone. Alloplastic bone grafting material includes bioactive glass, which promotes osteogenesis, and calcium phosphate-based materials like hydroxyapatite that are compositionally similar to natural bone, fostering new bone growth.
Bioactive glass displays high bioactivity, initiating reaction layers quickly upon implantation that facilitate rapid bone growth by attracting osteoblasts. Alloplastic grafts are particularly beneficial in surgeries for maxillary sinus elevation, periodontal defects, and bone crest augmentation, aiming to improve bone quantity and quality for dental implants.
Dental Bone Graft Procedure: Steps and Techniques

- Application of local anesthesia or sedation
- Making a small incision in the gum tissue
- Placing the bone graft material
- Possibly covering with a membrane for protection
- Repositioning the gum tissue
- Suturing the incision closed
Local anesthesia is commonly used to numb the treatment area, but general anesthesia or sedation may be recommended for more involved cases. After the procedure, any discomfort is typically controlled with pain relief medicine.
Material integration and osseointegration depend on the type of material used and the method of graft placement, without a consensus on the optimal timing.
Recovery from a dental bone graft allows patients to return home the same day, with healing taking anywhere from four to six months or more, which varies based on the individual’s healing capabilities and the procedure’s complexity.
Pre-Procedure Assessment
Prior to the bone graft procedure, the dental professional carries out an exhaustive pre-procedure evaluation. This starts with a detailed review of the patient’s dental and medical history to identify any conditions or medications that might impact the surgery or healing process.
An oral examination including the health of teeth, gums, and jaw is conducted alongside an evaluation of the patient’s oral hygiene and periodontal health to determine their suitability for a bone graft. The use of imaging, such as dental X-rays or scans, is integral to the assessment, aiding in the formulation of a personalized treatment plan that is discussed with and finalized by the patient.
Surgical Procedure
The surgical procedure for dental bone grafts follows a meticulously planned process. Here are the steps involved:
- Administer local anesthesia.
- Make an incision in the gum tissue at the bone graft site to expose the underlying bone.
- Place the bone graft material (autograft, allograft, xenograft, or alloplast) into the exposed site.
- Secure the graft with screws, wires, or pins if needed.
After the placement of the bone graft, the following steps are taken:
- The gum tissue is repositioned.
- The incision is closed with stitches or staples, which will be removed or dissolve over time.
- In some cases, a membrane may be applied over the bone graft to protect from soft tissue ingrowth and promote bone regeneration.
Recovery and Healing
After undergoing a bone grafting procedure, the healing and integration phase typically spans 4 to 9 months, contingent upon individual factors and the specific type of graft implemented. Most patients experience minimal pain post-surgery, which can be managed with prescribed medications or over-the-counter pain relievers.
Swelling and bruising can be reduced by applying ice packs to the face, keeping the head elevated, and using warm compresses as needed after the initial 48 hours. Post-operative recovery includes dietary modifications, maintaining oral hygiene, avoiding certain activities, and regular follow-up appointments to monitor the graft’s healing process.
When is Bone Grafting Necessary? Indications and Applications

- Maintain space for future implants or dentures
- Prevent bone loss within the empty socket
- Rebuild inadequate bone structure, especially in cases of significant alveolar bone loss
- Increase bone height in the upper jaw to ensure the stability of posterior implants
In preparation for dental implants, dental bone graft surgery may be employed as a form of bone grafting.
Bone grafts also play a vital role in the treatment of advanced periodontal disease. They help regenerate lost bone around teeth, reducing tooth mobility and the likelihood of tooth loss. Jawbone ridge reconstruction, which provides the necessary foundation and fit for dentures, can also be achieved with ridge augmentation and guided tissue regeneration via bone grafting.
Factors such as:
- previous tooth extractions
- gum tissue disease
- trauma
- smoking
can lead to jawbone deterioration, increasing the likelihood of needing a bone graft before further dental procedures like implants.
Potential Risks and Complications of Dental Bone Grafting
Like all surgical procedures, dental bone grafting carries potential risks and complications. While infections are rare, they can occur and may warrant the removal of the graft if an infection arises. To prevent infections, antibiotics are often prescribed, and patients are usually advised to complete the full course to prevent resistance.
Habits such as smoking can greatly reduce the success rate of bone grafts by increasing the risk of infection and failure. Bone graft failure, though relatively rare, can occur, particularly in smokers or those with specific medical conditions. There is also a risk of nerve damage during bone grafting, which can manifest as pain, numbness, or tingling, and damage to sensory and motor nerves can potentially result in complications like impaired speech and drooling.
Patients may also experience discomforts such as mild to moderate pain, bruising, and swelling after the procedure.
Post-Procedure Care and Maintenance
Post bone grafting procedure, adhering to specific post-operative care guidelines is vital for optimal healing. Patients generally report minimal discomfort and can manage any pain using pain relievers, which should be consumed with food to decrease the likelihood of nausea.
Post-surgery, patients must:
- Avoid vigorous mouth rinsing or spitting for several days
- Not disturb the graft site during gentle tooth brushing
- Follow specific instructions for wearing oral appliances like dentures or flippers
- Consume a soft and nutritionally balanced diet for a few days, with a gradual return to a normal diet as the surgical site heals.
Patients should monitor for symptoms such as swelling, bruising, and the occasional discharge of small granules from the graft site, using cold and warm compresses as needed and ensuring proper placement of gauze pads to control heavy bleeding.
Cost of Dental Bone Grafts: Factors and Saving Tips
The expense attached to dental bone grafting can vary between $200 to $3,000 per graft site, determined by several factors including the type of grafting material, geographical location, and the expertise of the dental professional. Synthetic graft options are generally less expensive compared to autogenous bone grafts or allografts.
Patients can explore various options to save on bone grafting, such as comparing dental practice prices, opting for services at dental schools, and discussing financing alternatives with the provider.
Despite the costs, dental bone grafting is a worthy investment for a healthy jawbone and a beautiful smile.
Alternative Options to Dental Bone Grafting
Although dental bone grafting is a prevalent method for reconstructing jawbone defects, there are alternative options as well. The All-on-4 implant method allows for immediate placement of implants with immediate cosmetic outcomes, even with significant bone loss.
Short implants provide an option that avoids bone grafting for patients with limited bone height. Zygomatic implants, anchored in the cheekbone, offer a graftless option suitable for patients with significant upper jaw bone loss, achieving a higher success rate than implants placed in grafted bone. However, patients considering zygomatic implants may need to travel to find a surgeon with expertise in this specialized procedure.
Summary
Dental bone grafting is a critical procedure that aids in the successful placement of dental implants, maintaining oral health, and expanding treatment possibilities. The procedure, though complex, is marked by high success rates and comes in several types to cater to unique patient needs. Despite potential risks and complications, proper post-procedure care and maintenance can ensure optimal healing and integration. With a range of cost factors and saving options, along with alternatives, every patient can find a suitable path to a healthy jawbone and a radiant smile.
Frequently Asked Questions
How painful are dental bone grafts?
Dental bone grafts are not very painful during the procedure, as they are done under anesthesia. After the procedure, there may be some swelling, bruising, bleeding, and mild discomfort once the anesthesia wears off.
What is the downside of bone graft?
The downside of bone grafting is that it may necessitate an additional operation, leading to a more painful recovery due to multiple surgery sites and limitations for major grafting procedures. Therefore, it is not ideal for extensive bone reconstruction.
How long do dental bone grafts take to heal?
Dental bone grafts can take between three and nine months to fully heal. Your recovery time will depend on factors such as the type of graft and your body’s healing capacity.
Why would a dentist need to do a bone graft?
A dentist would need to do a bone graft when a patient lacks sufficient bone tissue to support teeth or implants, often due to past gum disease or dental implant surgery. It helps to ensure the success of dental implants or other tooth restoration procedures.
What is a dental bone graft?
A dental bone graft is a procedure that rebuilds jawbone defects to provide strong support for dental implants when there’s not enough bone present. It’s necessary when insufficient bone would otherwise not support an implant.